
Diabetes is a common chronic medical condition that leads to increased blood sugar (glucose) levels. Severe complications can come from diabetes, including heart disease, vascular (blood vessel) disease and poor circulation, blindness, kidney failure, poor healing, stroke, and other neurological (nerve) diseases. Diabetes cannot be cured but can be successfully treated. Complications from diabetes can be prevented with careful blood sugar management and control of high blood pressure and high cholesterol levels when present.
PHYSIOLOGY:
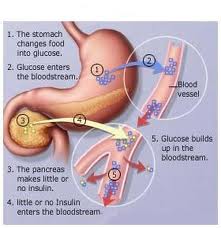
In diabetes the elevated blood sugar (glucose) levels are due to absolute or relative insufficiencies of insulin, a hormone produced by the pancreas. Insulin is a hormone that is involved in regulating how the body converts sugar (glucose) into energy. It normally works in the following way:
- During and immediately after a meal, digestion breaks carbohydrates down into sugar molecules (of which glucose is one) and proteins into amino acids.
- Right after the meal, glucose and amino acids are absorbed directly into the bloodstream, and blood glucose levels rise sharply. (Glucose levels after a meal are called postprandial levels.)
- The rise in blood glucose levels signals important cells in the pancreas, called beta cells, to secrete insulin, which pours into the bloodstream. Within 10 minutes after a meal insulin rises to its peak level.
- Insulin then enables glucose to enter cells in the body, particularly muscle and liver cells. Here, insulin and other hormones direct whether glucose will be burned for energy or stored for future use.
- When insulin levels are high, the liver stops producing glucose and stores it in other forms until the body needs it again.
- As blood glucose levels reach their peak, the pancreas reduces the production of insulin.
- About 2 – 4 hours after a meal both blood glucose and insulin are at low levels, with insulin being slightly higher. The blood glucose levels are then referred to as fasting blood glucose concentrations.
TYPES OF DIABETES:
 |
 |
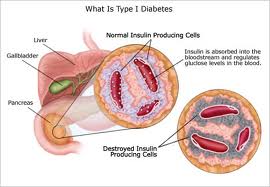
- Type 1 diabetes, often referred to as “juvenile” diabetes or “insulin-dependent” diabetes, occurs when the body’s pancreas does not produce enough insulin (the hormone that processes glucose). Type 1 diabetes is usually diagnosed in childhood or adolescence and requires lifelong insulin treatment.
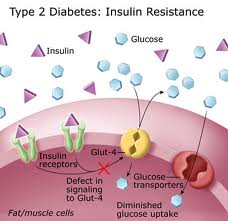
- Type 2 diabetes, also called “adult-onset” diabetes, is much more common. Type 2 diabetes is becoming more and more common in children and teenagers because of the increase in obesity in young people. Insulin resistance is a major issue in type 2 diabetes—the body produces insulin but is unable to process glucose appropriately. However, people with type 2 diabetes also have insulin deficiency, although not to the same degree as individuals who have type 1 diabetes.
SIGNS AND SYMPTOMS:
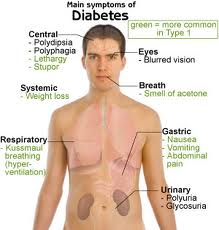
Typical symptoms of diabetes include excessive thirst, fatigue, frequent illness or infections, poor circulation (including tingling or numbness in the feet or hands), wounds that do not heal, blurred vision, and unintentional weight loss. Many people with type 2 diabetes have no symptoms, and it is discovered after testing for other medical problems or through screening in persons at high risk of developing type 2 diabetes.
DIET:
There is no such thing as a single diabetes diet. Patients should meet with a professional dietitian to plan an individualized diet within the general guidelines that takes into consideration their own health needs. General dietary guidelines for diabetes recommend:
- Carbohydrates should provide 45 – 65% of total daily calories. The type and amount of carbohydrate are both important. Best choices are vegetables, fruits, beans, and whole grains. These foods are also high in fiber. Patients with diabetes should monitor their carbohydrate intake either through carbohydrate counting or meal planning exchange lists.
- Fats should provide 25 – 35% of daily calories. Monounsaturated (such as olive, peanut, canola oils; and avocados and nuts) and omega-3 polyunsaturated (such as fish, flaxseed oil, and walnuts) fats are the best types. Limit saturated fat (red meat, butter) to less than 7% of daily calories. Choose nonfat or low-fat dairy instead of whole milk products. Limit trans-fats (such as hydrogenated fat found in snack foods, fried foods, and commercially baked goods) to less than 1% of total calories.
- Protein should provide 12 – 20% of daily calories, although this may vary depending on a patient’s individual health requirements. Patients with kidney disease should limit protein intake to less than 10% of calories. Fish, soy, and poultry are better protein choices than red meat.
- Lose weight if body mass index (BMI) is 25 – 29 (overweight) or higher (obese).

Several different dietary methods are available for controlling blood sugar:
- Diabetic exchange lists (for maintaining a proper balance of carbohydrates, fats, and proteins throughout the day)
- Carbohydrate counting (for tracking the number of grams of carbohydrates consumed each day)
- Glycemic index (for tracking which carbohydrate foods increase blood sugar)
MONITORING:
Both low blood sugar (hypoglycemia) and high blood sugar (hyperglycemia) are of concern for patients who take insulin. It is important, therefore, to monitor blood glucose levels carefully. Patients should aim for the following measurements:
- Pre-meal glucose levels of 70 – 130 mg/dL.
- Post-meal glucose levels of less than 180 mg/dL.
- Hemoglobin A1C Test: Hemoglobin A1C is measured every 3 months, or at least twice a year, to determine the average blood-sugar level. It shows how well blood sugar has been controlled over the period of several months. For most people with well-controlled diabetes, A1C levels should be at around 7%.
WARNING SIGNS OF HYPOGLYCEMIA:

Hypoglycemia (low blood sugar) occurs when blood sugar (glucose) levels fall below normal. Patients with type 1 diabetes should be aware of these symptoms of hypoglycemia: Sweating, Trembling, Hunger, Rapid heartbeat and Confusion.
It is important to quickly treat hypoglycemia and raise blood sugar levels by eating sugar, sucking on hard candy, or drinking fruit juice. Patients who are at risk for hypoglycemia should carry some sugar product, or an emergency glucagon injection kit, in case an attack occurs.
In rare and worst cases, hypoglycemia can lead to coma and death. Regular blood sugar monitoring throughout the day can help you avoid hypoglycemia. Patients are also encouraged to wear a medical alert ID bracelet or necklace that states they have diabetes and that they take insulin.
TREATMENTS:
- Insulin is always required to treat type 1 diabetes.
- Good nutrition, daily physical exercise, smoking cessation, and monitoring of blood sugar along with regular monitoring of hemoglobin A1C (a measure of long-term blood glucose control) are cornerstones of treatment for both type 1 and type 2 diabetes.
- In type 2 diabetes, oral medications should be prescribed if diet and exercise do not make improvements in blood sugar control after a few months. There are several types of medications used to treat type 2 diabetes; treatment is individualized based on each person’s medical needs.
- Insulin may be required to treat type 2 diabetes if diet, exercise, and oral medications do not improve blood glucose control. As in type 1 diabetes, this requires careful blood sugar monitoring to avoid hypoglycemia (extremely low blood sugar levels) and to optimize insulin dosing.
ORAL ANTIDIABETICS:
 |
 |
 |
Six kinds of diabetes medicine are available in pill form:
- Sulfonylureas (some brand names: Amaryl, DiaBeta, Diabinese, Dymelor, Glucotrol, Glucotrol XL, Glynase, Micronase, Orinase, Tolinase) are the most commonly prescribed diabetes medicines. These medicines help your body make insulin. They are inexpensive and have few side effects. Side effects may include weight gain and low level of sodium in the blood. Sulfonylureas can be taken alone or with metformin (a glucosidase inhibitor), pioglitazone (a thiazolidinedione) or insulin. If you’re allergic to sulfa, you can’t take a sulfonylurea.
- Metformin (brand name: Glucophage) may be prescribed for people who have diabetes and are overweight, because it may help with weight problems. Metformin helps the body use insulin better. Metformin can cause side effects such as nausea or diarrhea in some people. It can be taken with a sulfonylurea.
- Thiazolidinediones: rosiglitazone (brand name: Avandia) and pioglitazone (brand name: Actos). An older medicine, troglitazone (brand name: Rezulin) is no longer available because of the risk of liver problems. Rosiglitazone and pioglitazone appear less likely to cause liver problems, but people taking them need periodic liver tests. Other side effects may include weight gain and fluid retention. These medicines help your body respond better to insulin. Rosiglitazone and pioglitazone can be used alone or in combination with other diabetes medicines.
- Glucosidase inhibitors (brand names: Precose, Glyset) work in your stomach and bowels to slow down the absorption of sugar. This medicine can cause stomach pain, diarrhea and bloating, so it may not be a good choice if you have a history of stomach or bowel trouble. It can be taken alone or with a sulfonylurea.
- Meglitinides: Repaglinide (brand name: Prandin) is taken with meals to control your blood sugar. Your doctor can tell you how to adjust the dose according to the number of meals you eat. Repaglinide can be taken alone or with metformin. Nateglinide (brand name: Starlix) is taken with meals to keep your blood sugar level from getting too high after you eat. Side effects may include weight gain. Nateglinide can also be taken alone or with metformin.
- DPP-4 Inhibitors (Gliptins): Incretin mimetics belong to a new class of drugs that help improve blood sugar control. Incretins include glucagon-like peptide-1 (GLP-1) inhibitors and DDP-4 inhibitors. Dipeptidyl peptidase-4 (DPP-4) inhibitors, also called gliptins, are the second class of incretin drugs. They include sitagliptin (Januvia) and saxagliptin (Onglyza). They can be used alone or in combination with another oral diabetes drug (metformin, thiazolidinediones, or sulfonylureas). Janumet is a two-in-one pill that combines sitagliptin with metformin. DPP-4 inhibitors work in a similar way to GLP-1 inhibitors. However, unlike exenatide, which is given by injection, DPP-4 inhibitor drugs are taken as pills by mouth. Like GLP-1 inhibitors, DPP-4 inhibitors do not cause weight gain, have low risks for hypoglycemia, and have few severe side effects. The most common side effects include upper respiratory tract infection, sore throat, and diarrhea. Sitagliptin has been linked to cases of acute pancreatitis (inflammation of the pancreas). Patients should be monitored for signs of pancreatitis after treatment begins or the dosage is increased.
Your doctor may prescribe a combination of 2 or even 3 types of medicine to help control your blood sugar levels. Some combinations are available together in one pill. Some of these include a combination of a thiazolidinedione and a biguanide (Avandamet and ACTOplus Met) or a sulfonylurea and a biguanide (Glucovance and Metaglip).
INJECTABLE INCRETINS:

- GLP-1 Inhibitors (Exenatide and Liraglutide)
Incretin mimetics belong to a new class of drugs that help improve blood sugar control. Incretins include glucagon-like peptide-1 (GLP-1) inhibitors and DDP-4 inhibitors. GLP-1 inhibitors are given by injection and are prescribed for patients with type 2 diabetes who have not been able to control their glucose with metformin or a sulfonylurea drug. They can be taken in combination with these drugs or alone. - In 2005, the FDA approved exenatide (Byetta), the first GLP-1 inhibitor drug. Exenatide is a synthetic version of the hormone found in the saliva of the Gila monster, a venomous desert lizard. Exenatide is injected twice a day, 1 hour before morning and evening meals. In 2010, the FDA approved liraglutide (Victoza), a once-daily injectable GLP-1 inhibitor.
- Side Effects. These drugs stimulate insulin secretion only when blood sugar levels are high and so have less risk for causing low blood sugar (hypoglycemia) when it is taken alone. However, the risk for hypoglycemia increases when GLP-1 inhibitors are taken along with a sulfonylurea drug. There does not appear to be a risk for hypoglycemia when they are used along with metformin. Other side effects may include nausea, vomiting, and diarrhea.
- Exenatide and liraglutide have been associated with cases of acute pancreatitis, which is sudden inflammation of the pancreas. Symptoms of acute pancreatitis include severe abdominal pain that may radiate to the back. The pain may or may not be accompanied by nausea and vomiting. Patients who feel severe stomach pain that does not go away should seek prompt medical attention. Exenatide may cause new or worse problems with kidney function, including kidney failure. It should not be used by patients with severe kidney problems.
INSULINS:
 |
 |
Insulin lowers blood sugar by allowing it to leave the bloodstream and enter cells. Not everyone needs insulin. People with type 1 diabetes can’t make their own insulin. They must take insulin every day. Insulin is usually injected under the skin. In some cases, a pump delivers the insulin continuously. Insulin does not come in pill form.
Insulin preparations differ in how fast they start to work and how long they last. The health care professional will review your blood glucose levels to determine the appropriate type of insulin you should use. More than one type of insulin may be mixed together in an injection to achieve the best blood glucose control.
Components of insulin administration:
- Basal insulin administration. The basal component of the treatment attempts to provide a steady amount of background insulin throughout the day. Basal insulin levels maintain regular blood glucose needs. Insulin glargine now offers the most consistent insulin activity level, but other intermediate and long-acting forms may be beneficial when administered twice a day. Short-acting insulin delivered continuously using a pump is proving to a very good way to provide basal rates of insulin.
- Mealtime insulin administration. Meals require a boost (a bolus) of insulin to regulate the sudden rise in glucose levels after a meal.
Types of Insulin:
Insulin cannot be taken orally because the body’s digestive juices destroy it. Injections of insulin under the skin ensure that it is absorbed slowly by the body for a long-lasting effect. The timing and frequency of insulin injections depend upon a number of factors:
- The duration of insulin action. Insulin is available in several forms, including: standard, intermediate, long-acting, and rapid-acting.
- Amount and type of food eaten. Ingestion of food makes the blood glucose level rise. Alcohol lowers levels. The person’s level of physical activity. Exercise lowers glucose levels.
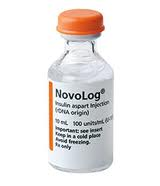
Fast-Acting Insulin: Insulin lispro (Humalog) and insulin aspart (Novo Rapid, Novolog) lower blood sugar very quickly, usually within 5 minutes after injection. Insulin peaks in about 4 hours and continues to work for about 4 more hours. This rapid action reduces the risk for hypoglycemic events after eating (postprandial hypoglycemia). Optimal timing for administering this insulin is about 15 minutes before a meal, but it can also be taken immediately after a meal (but within 30 minutes). Fast-acting insulins may be especially useful for meals with high carbohydrates.
Regular Insulin: Regular insulin begins to act 30 minutes after injection, reaches its peak at 2 – 4 hours, and lasts about 6 hours. Regular insulin may be administered before a meal and may be better for high-fat meals.
Intermediate Insulin: NPH (neutral protamine Hagedorn) insulin has been the standard intermediate form. It works within 2 – 4 hours, peaks 4 – 12 hours later, and lasts up to 18 hours. Lente (insulin zinc) is another intermediate insulin that peaks 4 – 12 hours and lasts up to 18 hours.
Long-Acting (Ultralente) Insulin: Long-acting insulins, such as insulin glargine (Lantus), are released slowly. Long-acting insulin peaks at 10 hours and lasts up to 20 hours.

Combination: Regimens generally include combinations of short and longer-acting insulins to help match the natural cycle. For example, one approach in patients who are intensively controlling their glucose levels uses 3 injections of insulin, which includes a mixture of regular insulin and NPH at dinner. Another approach uses 4 injections, including a separate short-acting form at dinner and NPH at bedtime, which may pose a lower risk for nighttime hypoglycemia than the 3-injection regimen.
Insulin Pens: Insulin pens, which contain cartridges of insulin, have been available for some time. Until recently, they were fairly complicated and difficult to use. Newer, prefilled pens (Humulin Pen, Humalog) are disposable and allow the patient to dial in the correct amount.
